You may have recently been seen in the Emergency Department or by a neurologist and told you have Parsonage-Turner Syndrome (PTS) — also known as Neuralgic Amyotrophy or Brachial Neuritis. It’s a mouthful, and naturally, you might feel overwhelmed, especially if this came out of nowhere.
You’re not alone. This condition can be painful, confusing, and frustrating — but recovery is possible, and there’s a clear path forward. Let’s walk through what this condition is, why it happens, how we diagnose it, and most importantly, how we can help you regain strength and function.
🧠 What Is Parsonage-Turner Syndrome?
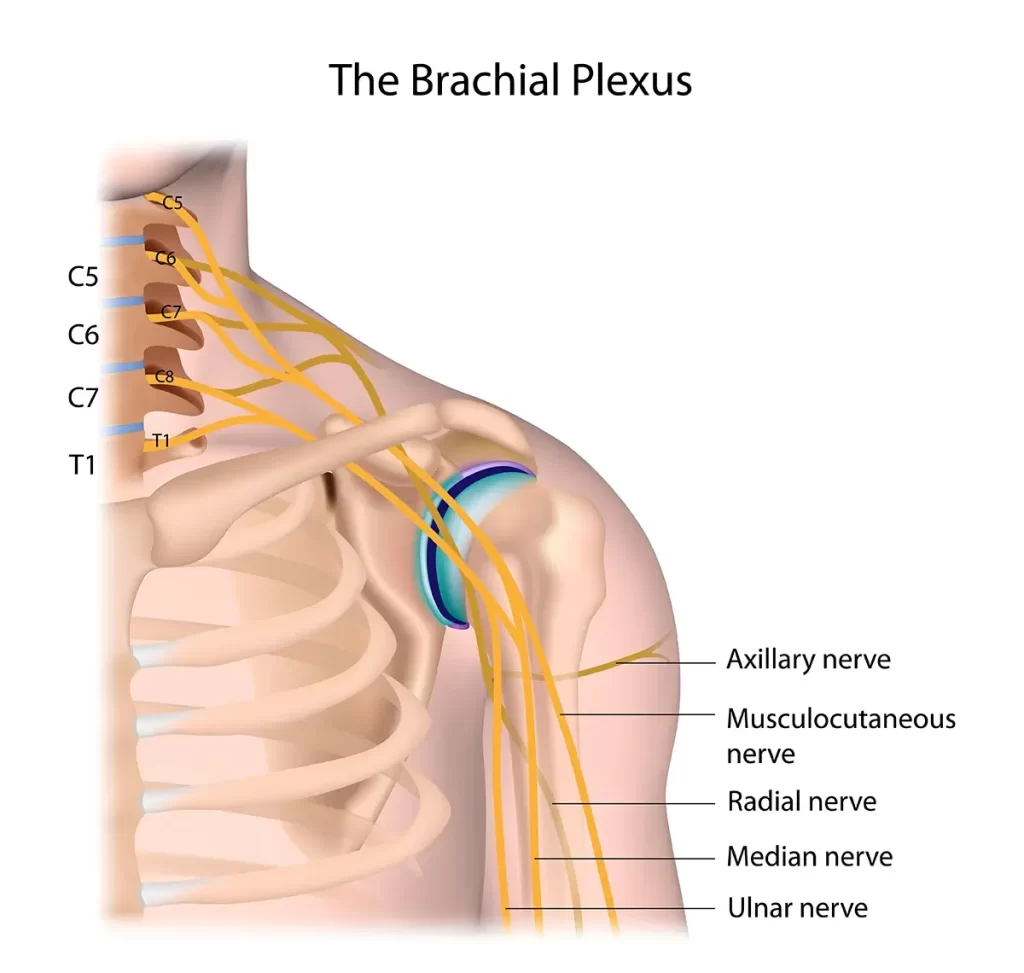
Parsonage-Turner Syndrome is a rare neurological condition that affects the brachial plexus — the network of nerves that controls movement and sensation in your shoulder, arm, and hand.
It’s essentially a form of nerve inflammation (neuritis) that leads to:
- Sudden, intense pain (often unrelenting)
- Muscle weakness
- Loss of function
- In some cases, visible muscle wasting or shoulder blade winging
While the condition is usually self-limiting, recovery can take months to years and often requires targeted rehabilitation.
🔎 What Causes It?
In most cases, the exact trigger is unknown — this is called idiopathic Parsonage-Turner Syndrome.
But common patterns and risk factors include:
- Viral infections (e.g. influenza, COVID-19)
- Recent vaccinations
- Surgery (especially in the neck or shoulder region)
- Autoimmune reactions
- Intense physical exertion or trauma
- Stress or immune suppression
There’s also a hereditary form called Hereditary Neuralgic Amyotrophy (HNA) — caused by a genetic mutation. This is much rarer and often presents earlier in life, with recurring episodes.
⚠️ Common Signs and Symptoms
PTS typically presents in two stages:
🔥 Phase 1: Sudden Severe Pain
- Often described as burning, stabbing, or electric
- Usually deep in the shoulder, but may involve the neck, upper arm, or scapula
- Unrelenting, worse at night, and not responsive to standard pain medications
💪 Phase 2: Weakness and Muscle Wasting
- Pain begins to settle, but profound weakness sets in
- Difficulty lifting the arm, reaching overhead, or performing fine motor tasks
- Visible muscle atrophy (shrinking)
- Scapular winging if the long thoracic or spinal accessory nerve is involved
- Numbness or tingling may also occur, but is less prominent
The affected muscles depend on which nerves are inflamed — commonly:
- Suprascapular nerve → infraspinatus/supraspinatus weakness
- Long thoracic nerve → serratus anterior and winged scapula
- Axillary nerve → deltoid and shoulder abduction issues
- Anterior interosseous nerve → thumb/index grip weakness
🧪 How Is It Diagnosed?
Parsonage-Turner Syndrome is a clinical diagnosis supported by advanced imaging and nerve testing. Most patients present acutely and are evaluated in the Emergency Department, with referral to neurology or peripheral nerve specialists.
Here’s the step-by-step breakdown:
🧑⚕️ Clinical Assessment
- History of sudden, severe shoulder/arm pain followed by weakness
- Often non-traumatic
- Clear temporal sequence of events
- Unusual muscle pattern or scapular winging may be present
🔬 Imaging and Tests
1. MRI of the Shoulder or Cervical Spine
- Rules out rotator cuff tear, disc herniation, tumors, or compressive pathology
- May show muscle edema or denervation changes
2. MRI of the Brachial Plexus
- Common in hospital settings
- May reveal nerve swelling or inflammation
- Confirms diagnosis and rules out structural mass lesions
3. MR Neurography
- High-resolution imaging of nerve fascicles
- Often reveals hourglass constrictions — a focal “pinching” within the nerve, without external compression
- Seen in up to 85% of idiopathic PTS cases
- Supports the theory of immune-mediated fascicular torsion or internal scarring
4. High-Resolution Ultrasound
- A non-invasive tool to visualise:
- Hourglass constrictions
- Nerve swelling
- Muscle denervation
- Requires specialist skill
5. Nerve Conduction Studies (NCS) & Electromyography (EMG)
- Helps identify which nerves are involved
- Detects signs of nerve degeneration and regeneration
- Most useful after 2–3 weeks from symptom onset
6. Blood Tests
- Rule out autoimmune, infectious, or metabolic mimics (e.g. diabetes, vasculitis)
💉 What About Injections?
In select cases — particularly in the acute phase — a short course of oral corticosteroids (e.g. prednisone) may reduce nerve inflammation and shorten the pain phase. Evidence is limited but suggests early initiation may help.
There have also been case reports of:
- Ultrasound-guided brachial plexus injections (local anaesthetic + steroid)
- These may offer pain relief, especially in severe cases, but are not routine first-line care
- Typically reserved for hospital or interventional pain settings
🧭 What’s the Usual Treatment Approach?
There’s no “cure,” but most patients gradually recover. Management is based on the phase of the condition:
✅ Phase 1: Pain Management
- Corticosteroids (if early enough)
- Nerve-specific pain relief: pregabalin, amitriptyline, duloxetine
- Ice, positioning, activity modification
- Avoid overloading the weak limb
✅ Phase 2: Recovery and Rehabilitation
- Begins once pain improves and weakness becomes evident
- This is where physiotherapy plays a crucial role
🧠 Role of Physiotherapy
Once the acute inflammation settles, your biggest challenges are:
- Loss of strength
- Impaired coordination
- Altered scapular control
- Difficulty with functional tasks (lifting, driving, work)
Here’s how physiotherapy helps:
🔄 1. Restore Movement and Prevent Stiffness
- Gentle range of motion exercises to prevent frozen shoulder
- Mobilisation of adjacent joints to compensate temporarily
🦴 2. Improve Stability with Supportive Devices
- Scapular bracing can help if scapular winging is severe or causes instability
- It provides external support, reduces winging, and improves confidence during movement
- Used temporarily while nerve recovery begins
⚡ 3. Electrical Muscle Stimulation (EMS)
- Helpful for muscles that can’t yet contract voluntarily
- Especially for:
- Infraspinatus/supraspinatus (posterior cuff)
- Serratus anterior (scapular control)
- Deltoid (axillary nerve recovery)
- May reduce pain and improve shoulder stability early in rehab
🧩 4. Strengthening and Re-Education
- Begin with low-load, nerve-specific strengthening
- Progress to compound functional movements as recovery allows
- Monitor for compensatory overuse of unaffected muscles
🛡️ 5. Functional and Occupational Integration
- Gradual return to work, driving, and recreational activity
- Task-specific rehab
- Support for long-term adaptations if needed
⏳ What’s the Prognosis?
- Most patients recover partially or fully within 12–24 months
- Some nerve branches recover faster than others
- If hourglass constrictions persist, recovery may plateau — and referral to a peripheral nerve surgeon may be considered in very select cases
👨⚕️ A Word From Me
Parsonage-Turner Syndrome is a rare condition, and understandably, most people — including many physiotherapists — may not have encountered it before. That uncertainty can make the journey even more isolating.
Fortunately, I’ve had the opportunity to work with a handful of patients recovering from PTS in the past. Many were scared, frustrated, and unsure whether they’d ever regain full function. But with the right support, a structured rehab plan, and careful pacing, I’ve seen people return to lifting, playing with their kids — and doing the things that matter most.
You don’t have to figure this out alone.
📍 Need Help With Parsonage-Turner Syndrome?
At Melbourne Shoulder Rehab, we specialise in managing complex shoulder and nerve-related conditions like PTS. If you’re recovering from brachial neuritis or feeling stuck in your rehab — we’re here to guide you with clarity, structure, and evidence-based care.
👉 Book your consultation today and let’s start rebuilding your strength, movement, and confidence.
